News Team member Stephanie Oehler describes how the online "trad-wife" aesthetic fuels the flames of the anti-vaccination movement during the second-largest measles outbreak of the 21st century.
Understanding the Impact of Rural Hospital Closures Across the United States
As hospitals close, travel times for care increase, outcomes worsen, and maternal and child care crashes. Do solutions exist?
By Caroline Hansen
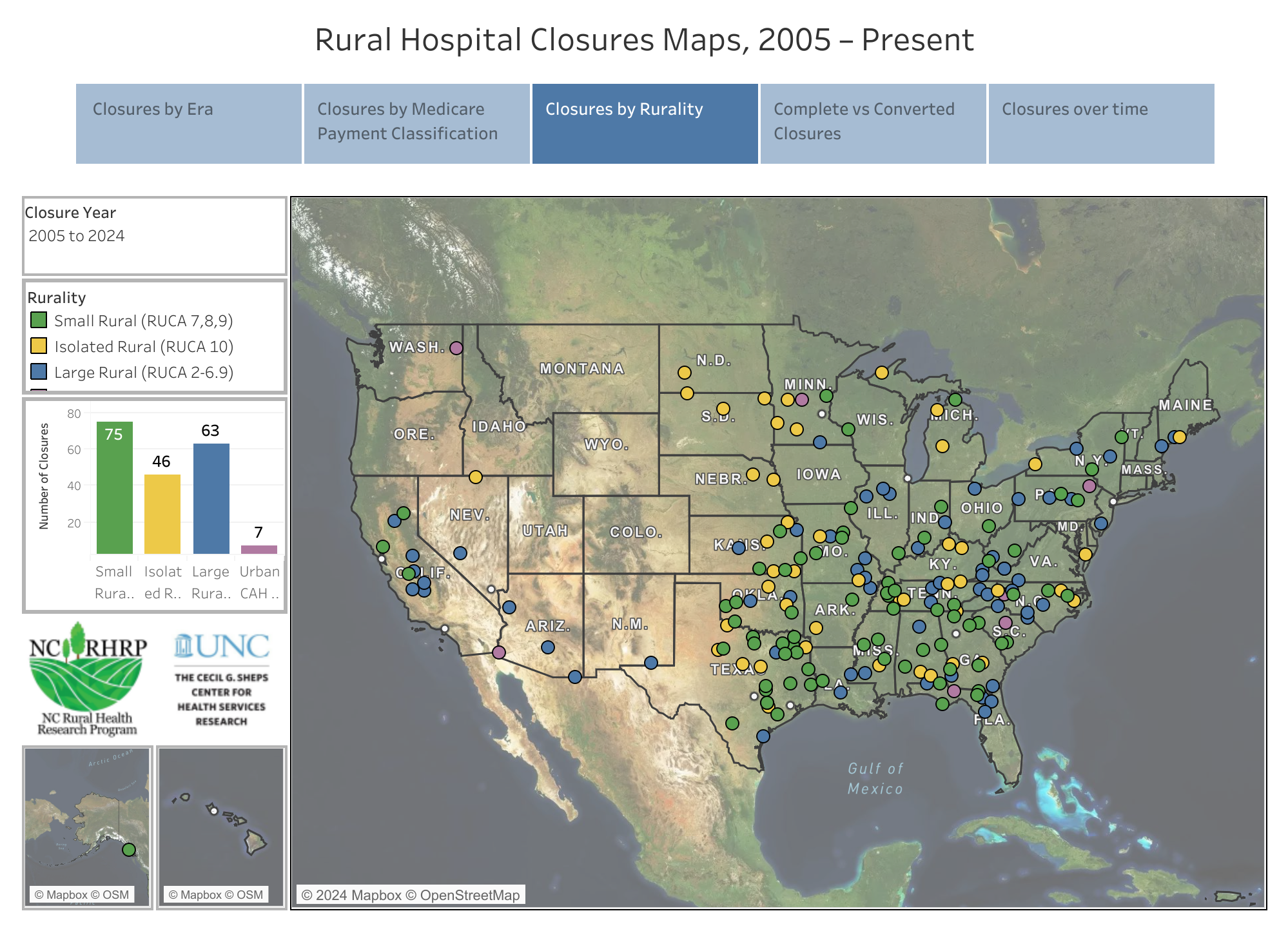
Across the United States, hospitals that serve rural areas are closing — 136 between 2010 and 2021, according to the American Hospital Association. It’s a trend that threatens to deprive rural residents of reliable health care, as well as risk the safety of pregnant women who must drive longer distances for maternity care and delivery. There are over 1,000 small rural hospitals. This makes up almost a fourth of short-term general hospitals in the country but only receives 2 percent of total national hospital spending.
Statistics make the problem clear: The south and southeastern regions are at higher risk. In the south, 10 percent of rural counties lost one or more hospitals between 2007 and 2018. Close to half of these closures left the county without a hospital. Georgia has the 7th most rural hospital closures since 2005. This highlights the crisis of rural health care. However, there are trends in why rural hospitals are closing.
Financial stress is the primary driver of rural hospital closures. Since rural populations have lower densities, their hospitals are plagued by low patient volumes. Lower patient volumes limit “risk pooling”. This is where healthier individuals and sick individuals go to the hospitals and the costs of the healthier individuals level out the costs of sicker individuals. Without the ability to risk pool, sicker individuals increase the operational costs that burden hospitals. Rural populations are also statistically older and sicker, which increases healthcare demand and costs. To compound costs, populations are more likely to be insured or rely on Medicare and Medicaid.
Financial Strain and Staffing Shortages
Reimbursement and Medicaid expansion is not their only challenge. Staffing shortages are impacting access to care, and have exponentially increased over the past four years. Rural populations have less access to health care services and receive less preventative care compared to urban populations. Without preventative care, patients are entering the hospital more frequently with worse conditions, increasing costs. In addition to not receiving preventive care, they are lacking physicians when they do seek care. Only 10 percent of physicians practice in rural areas, even though rural patients make up 14 percent of the population. This drought of physicians is visible, with 70 percent of primary care health professional shortage areas being located in rural areas.
Dr. Bush, a physician who has owned practices in Macon and Grey Georgia, describes his experience with struggling to recruit staff to work in nonmetropolitan areas. “Macon is good as far as primary care recruiting, but as far as getting specialists, it’s much harder to get a specialist to come to Macon than it is to come to Atlanta. And that has to do with call coverage. You don’t want to be the only pediatric orthopedic surgeon in Macon, you’re on call every night.”
Staffing shortages and the struggle to recruit new physicians, especially in specialty care, create a cyclical problem. Physicians do not want to be the sole physician in a rural area, but they cannot get any physicians to come in the first place.
How Closures Affect Rural Populations
With 14 percent of all Americans living in rural areas, this crisis is impacting a larger population of Americans. Health outcomes in rural areas have also been declining. Since 2019, rural adults have had higher rates of mortality due to heart disease, cancer, unintentional injury, and stroke in comparison to urban adults. These declining health outcomes can be correlated to significant shortages of healthcare services. With hospitals closing, 812,314 United States residents could no longer access a hospital within 15 minutes.

Rural hospital closures impact not only travel time but also health outcomes. Dr. Guldi is an Associate Professor of Economics at the University of Central Florida and a researcher in health economics and economics demography. She highlights the correlation between health outcomes and rurality, “The big takeaway is the degree of rurality is important when studying health outcomes.”
Research highlights that hospital closures worsened prenatal, infant, and delivery outcomes in moderately rural counties. In Georgia, nine rural labor and delivery units closed outside of the Atlanta Metropolitan area from 2012 to 2016. Research in the Maternal Child Health Journal, states that labor and delivery units that closed had a higher proportion of black female patients, black birthing parents, and patients insured by Medicaid. The impact of these closers increasingly impacts black and low-income women. With black women already facing higher maternal mortality and infant mortality rates, their risk compounds with hospital closures and access barriers.
Research spotlights the loss of maternity services in rural areas. Between 2004 and 2014, 9 percent of rural counties had their hospital’s maternity service closed, and 45 percent did not have any maternity services. With birthing and maternity units closing, this can leave rural areas with “maternity care deserts”.
How Federal Reimbursement Accidentally Makes This Problem Worse
To combat rurality causing declining health outcomes there are two programs from the Center for Medicare and Medicaid services in place to offset costs. These programs aim to address low reimbursement rates impacting financial stability, to prevent rural hospitals from closing.
These hospitals can be deemed “Medicare Dependent Hospitals”, which gives them a financial advantage in the Center for Medicare and Medicaid (CMS) reimbursement patent system called the prospective payment system. To be eligible for this designation a hospital has to be located in a rural area, have less than a hundred beds, and have more than 60 percent of their inpatient days or be discharged from Medicare beneficiaries.
In addition, to combat low patient volumes, there is an additional prospective payment adjustment for hospitals deemed “Low-Volume Hospitals”. To qualify, a hospital needs less than 3,800 discharges and be more than 15 miles from the nearest hospital.
While these programs work in protecting rural hospitals from closure, they are still struggling. For example, there are over 1,000 small rural hospitals. This makes up almost a fourth of short-term general hospitals in the country but only receives 2 percent of total national hospital spending. With rural hospitals providing the majority of the care for their area, they are receiving minimal funding, even with CMS’s programs.
A Snapshot of the Crisis in Georgia
In Georgia, 18 rural hospitals out of 30 are at risk of closing. Within these closures in Georgia, most counties have smaller populations with high minority presence. It is important to note that 74 percent of hospital closures occur in states that have not expanded Medicaid or have had Medicaid for less than a year. Rural areas are increasingly impacted by Medicaid expansion since individuals are less likely to have private insurance coverage and be uninsured. Rural areas have a 2 to 3 percent higher uninsured rate than urban areas. Medicaid expansion could aid in lowering rural uninsured rates. Research shows that Medicaid expansion is statistically significant in improving hospitals’ economic stability and lowering their risk of closure. Currently 41 states– including DC– have adopted Medicaid Expansion, with the majority of states declining expansion being located in the South. Highlighting the connection between the majority of rural hospital closures in the south and the states not expanding Medicaid in the south as well.

Seeking Solutions: Initiatives and Innovations to Prevent Closures
There is hope to fix staffing shortages and rural hospital closures. A great example is the Georgia Physicians for Rural Areas Assistance Program’s Donations for Rural Hospitals. This program assists in paying debt to practitioners who practice full-time in underserved, rural counties.
To financially support rural hospitals, Georgia created the “Georgia Rural Hospital Tax Credit Program”, also called Georgia HEART. Georgia HEART provides the option to receive a full state tax income credit for contributions to a designated Rural Hospital Organization. In 2023, Georgia HEART received over $72 million from Georgia taxpayers, to support the 54 hospitals in Georgia with a rural hospital designation.
The creation of programs to prevent closures and end staffing shortages is the first step to creating equitable health outcomes for rural communities. As previously stated, Medicaid Expansion can also improve hospital financing and prevent closures. Overall, rural health is in crisis, and the steps being taken to improve rural health can be instrumental. Supporting organizations and programs that assist rural hospitals can provide individuals with the ability to make their mark in bridging the rural and urban health outcomes gap.
