Manju Karthikeyan recommends "This Podcast Will Kill You" for engaging, relatable discussions on health topics, humanizing diseases with witty banter, and drink recipes, available on all streaming platforms.
Separating Hallucinogens and Hallucinations: How Psychedelics Could Be Modified to Treat Psychiatric Disorders
New research separates psychedelics’ hallucinogenic effects from their potential psychiatric benefits
By Katie Stachowicz
When most people think about psychedelic drugs, they might picture an hours-long high with trippy, colorful hallucinations. However, a rising branch of research suggests their active compounds could be effective as treatments for disorders from depression to substance use disorders. Even more exciting, scientists have recently figured out how to separate their hallucinogenic action from their potential clinical use, suggesting that more effective antidepressants could be in the works without dangerous side effects.
Using psychedelics to treat psychiatric disorders is no new phenomenon. The creation of lysergic acid diethylamide, more commonly known as LSD, in the 1930s led to an explosion of research that died down before slowly picking back up in the 1990s. However, until recently, LSD and other psychedelics like psilocybin (the active compound in psychedelic mushrooms) were believed to help with psychiatric disorders by activating serotonin receptors, a popular target of antidepressants for decades.
A new study from the University of Helsinki, published in June in Nature Neuroscience, suggests another possibility. Researchers found that psychedelics bind tightly to another receptor, TrkB (pronounced track-bee), in addition to serotonin receptors.
Why is this important? Well, it seems that binding to serotonin receptors causes hallucinations, but that antidepressant effects may instead come from binding to TrkB receptors.
“We found a high-affinity binding site for psychedelics,” says Plinio Casarotto, the current Deputy Editor at iScience and a co-author on the study. “Everything from there on out was to validate that.”
This is not to say that serotonin receptors aren’t involved in depression and other disorders – just that these TrkB receptors may be a lot more directly involved than scientists used to think. Turning on TrkB receptors helps brain cells form new connections between one another in a process called neuroplasticity. Most antidepressants don’t attack a depressive state directly, Casarotto explained; they help the brain form these new pathways. And psychedelics? They really open the brain up to change.

Finding treatment potential without the high
But the story doesn’t end there. Although specialized clinics in some countries have begun to use psychedelics for severe, untreatable depression, clinicians must monitor patients 24/7 because of the hallucinogenic side effects, making it very difficult to prescribe. This new study, along with a few others (see below), shows that hallucinations may come from how psychedelics interact with serotonin receptors, while antidepressant effects come from how they interact with TrkB. In both this study and a previous one, in a mouse with genetically modified serotonin receptors that couldn’t bind the psychedelic molecule, the mouse-equivalent hallucinatory side effects appeared to disappear, while neuroplasticity still occurred. However, when TrkB was mutated so it couldn’t bind to the psychedelic, the opposite happened: hallucination equivalents, but no neuroplasticity.
To sum up the results, you need TrkB for neuroplasticity, but not for hallucinations, and vice versa for serotonin receptors. This is a shocking idea to many psychedelic researchers.
“These ideas are new, the things we need to explore are new,” explains Praachi Tiwari, a postdoctoral researcher from the Center for Psychedelic and Consciousness Research at Johns Hopkins University School of Medicine who studies the therapeutic potential of psychedelics in treating mental health disorders. “I would love to see someone else somewhere else in the world replicate this study and then push it further. If it’s replicable, the field has a lot of potential to bridge [psychology and molecular signaling] together.”
While it’s still early for a total shift in focus, this discovery points to TrkB as a good target for more antidepressant research. There are a couple of different avenues. For one, scientists could change the structure of an existing psychedelic compound so that it would bind to TrkB, but not to serotonin receptors. Unfortunately, this will take years of testing and clinical trials to ensure safety. Alternatively, clinicians could administer psychedelics alongside a second compound that blocks binding to serotonin receptors to help activate TrkB and neuroplasticity without hallucinations. While still requiring clinical trials to make sure that the process was free of unwanted side effects (and that the psychedelics couldn’t be abused), this might be a band-aid that doctors could use before a more permanent solution was found through the typical process.
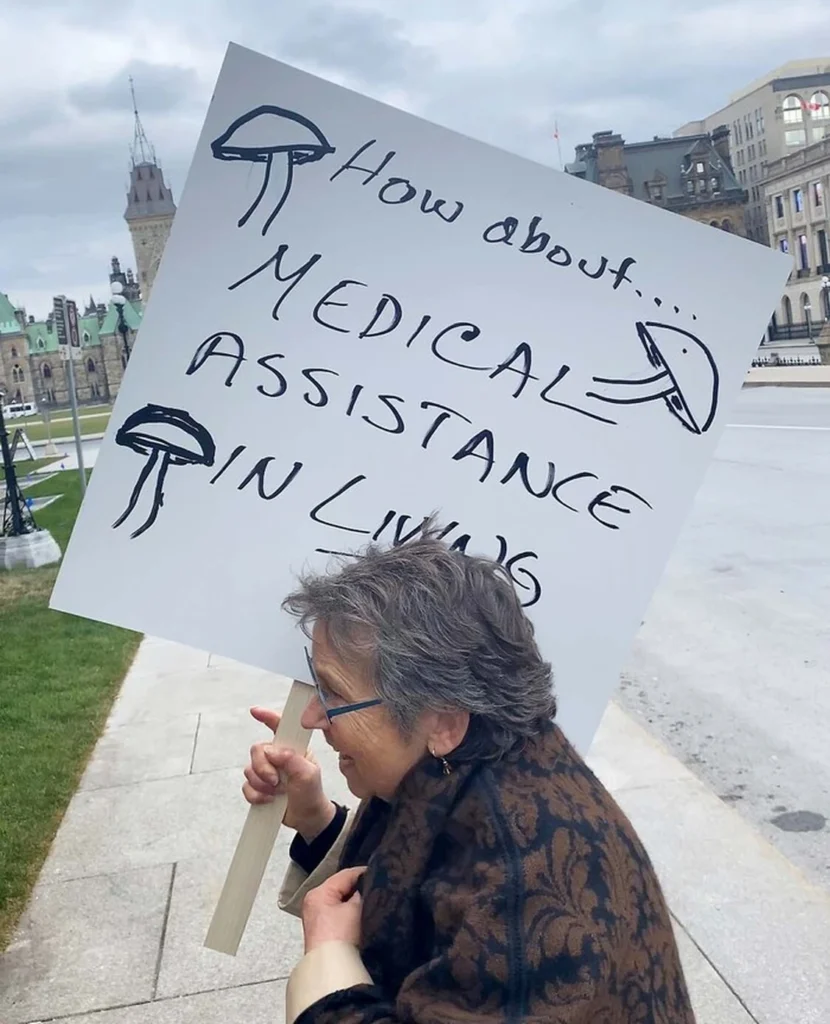
Tackling legal and ethical concerns
The concern for the abuse of these substances is a major barrier to their research and medicinal use. LSD and magic mushrooms are currently listed as Schedule I drugs in the United States alongside marijuana and ecstasy, meaning they have no medicinal value and a high potential for abuse. While many studies confirm their high potential for abuse, the lack of medicinal value is being called into question. Already, Colorado and Oregon have legalized the therapeutic and recreational use of mushrooms for those over the age of 21, and California may soon add itself to that list. Notably, though, doctors can’t give these compounds to patients. Instead, the patients need to go to a specialized “healing center.”
This is not a cure for depression, the authors warn, nor do they endorse using psychedelics in a clinical setting. While the study’s findings suggested that psychedelics could eventually serve as a basis for effective antidepressants, a lot more work needs to be done, including finding a molecule that would interact with TrkB receptors without interfering with serotonin receptors. And even a perfect drug wouldn’t be enough by itself — at the end of the day, patients still must work to set new mindsets for themselves.
“TrkB [activation] alone will not be sufficient,” says Eero Castrén, a research director at the University of Helsinki’s Neuroscience Center and another co-author of the paper. “It gives you the opportunity to make a change in your health, but for that to happen, you will have to demonstrate the change you want to happen. If you don’t produce activity by behaving, your brain has no guidance as to which networks and which connections to retain for better health and which to prune.”