New from the @EmoryCSHH News Team: As experts highlight the urgent need for an improved dengue vaccine, a new debate emerges about whether alcoholic beverages should carry cancer warning labels. Meanwhile, the author of "Anxious Generation" argues for granting children a "license to roam" to enhance their autonomy.
By: Jessica Maaskant
Cancer is an ever-evolving problem in our society. However, our treatments for cancer are constantly improving. Immunotherapies are a newer branch of these treatments that involve supporting the patient’s immune system in fighting cancer rather than solely relying on drugs, radiation, and surgery. [1] Immunotherapies are becoming more prevalent in treatment plans for patients due to the ability to personalize them to the patient. One such immunotherapy is the Chimeric Antigen Receptor T cell (CAR T) therapy. This treatment involves first taking out a patient’s own T cells which are immune cells that help kill cancer cells. Then these cells are taken to a lab where the genes are altered so the cells express B cell antigen receptors, which are receptors from immune cells that help recognize cancer cells. These receptors are designed to target the cancer that the patient has. Antigens are proteins that can be found on cancer surfaces, making them ideal targets for our immune cells. Doctors then reintroduce these altered T cells with antigen receptors into the patient to let the new immune cells get to work. [2]
Since 2017, 6 CAR T cell therapies have been FDA approved: Tisagenlecleucel (tisa-cel)/Kymriah, Axicabtagene ciloleucel (axi-cel)/Yescarta, Brexucabtagene autoleucel (brexu-cel)/Tecartus, Lisocabtagene maraleucel (liso-cel)/Breyanzi, Idecabtagene vicleucel (ide-cel)/Abecma, and Ciltacabtegene autoleucel (cilta-cel)/Carvykti. [3] These treatments are currently primarily used for patients with types of relapsed or refractory cancers. Relapsed cancers are ones that have been treated and returned, and refractory diseases are ones that have stopped responding to therapies altogether. In other words, CAR T is often used as a last resort against these stubborn cancers and has had great success. Patients who receive CAR T treatment have an improved survival rate of 30-40% and long-term survival is improving too. [4] The reason CAR T is only used as a last resort is largely due to the novelty of the therapy, as well as the cost and complexity of it. A single round of therapy can cost $373,000 to $475,000. [5] It is typically covered by medicare and some other insurances however the price makes it difficult for those who cannot get it covered to receive this treatment. [6] Over time, CAR T therapies will likely expand to other cancers, and as the barriers to this treatment are addressed, perhaps it will become implemented as an initial part of treatment plans.
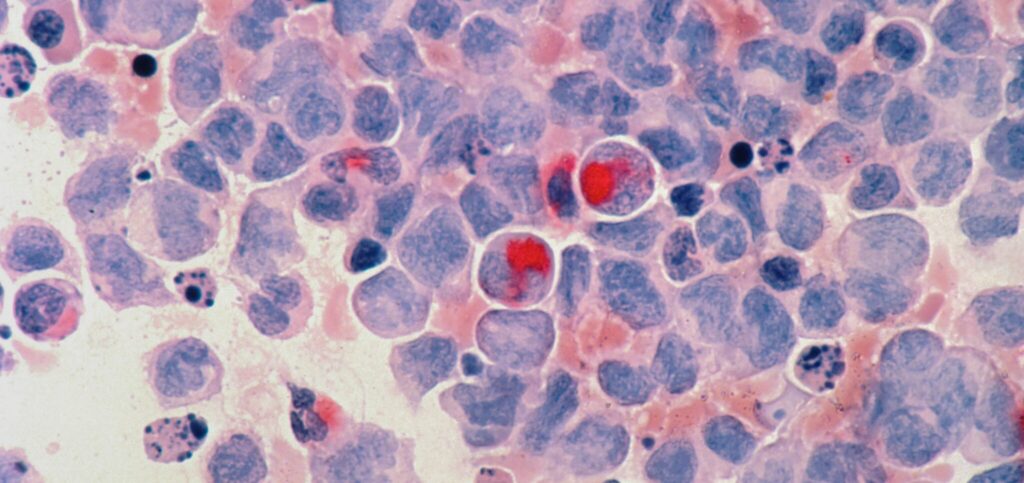
Currently, CAR T is most commonly used on refractory/relapsed B-cell lymphoma, acute lymphoblastic leukemia, and multiple myeloma. [7] All of these are cancers that affect the patient’s blood. Lymphomas originate in lymphocytes (white blood cells used to fight infection), leukemias originate in the blood and bone marrow, and myeloma begins in the blood plasma cells. [2] Due to the similar natures of these cancers, there has been a lot of focus on expanding CAR T cell applications for these cancers and other similar blood cancers.
Cilta-cel, the 6th type of CAR T, was approved by the FDA just this year on February 28, 2022. Cilta-cel targets a receptor known as B-cell maturation antigen (BCMA) which is a marker of Multiple Myeloma (MM) cells. BCMA is critical for the MM cells to survive so it is unlikely to mutate, meaning it is an ideal target for cancer therapies. [8] In a clinical trial for Cilta-cel in patients with advanced MM, 78% of patients were in complete remission almost 2 years after receiving one treatment and 98% of patients had some improvements with their cancer. [9] The FDA approved this treatment for patients with relapsed/refractory MM, and many are optimistic that it might become a primary treatment for these patients with particularly persistent MM.
There are some important side effects to be aware of with these CAR T cell therapies. First, patients need low-dose chemo before they are reinfused with the CAR T cells in order to help the CAR T cells survive and multiply in the patient. This means that these patients are at risk for all of the common chemo side effects like fatigue and increased risk of infection. [10] Serious side effects associated with the CAR T cells themselves are cytokine release syndrome, nervous system problems, and low blood counts. [2] With any new area of medicine, there are also often unexpected side-effects in humans that may not show up in vitro and in vivo studies. In 2021, in a 10 person clinical trial testing the efficacy of a new vector for CAR T cell therapy, the CAR T cells became cancerous in 2 of the patients. [11] The risks associated with CAR T cell therapies highlight the need to put more research/funding into this field of cancer therapeutics. In addition to developing novel CAR T cells, scientists are also looking for ways to maximize the benefits and minimize the risks associated with the current FDA-approved treatments.
The field of CAR T cell therapies has skyrocketed in the past decade. These treatments have changed how healthcare professionals are treating patients with relapsed B-cell lymphomas and Multiple Myeloma. However, the implications for these treatments don’t stop there. CAR T cells are a way to optimize the patient’s own immune system for fighting cancer. In the short timeframe that CAR T cells have been around, they have already drastically improved survival rates in patients. Immunotherapies are the future of cancer treatments, and new treatments like Cilta-cel are expected to continue growing our medical arsenal against some of the worst and most unrelenting forms of cancer.
References
[1] Immunotherapy for Cancer–National Cancer Institute (nciglobal,ncienterprise). (2015, April 29). [CgvArticle]. https://www.cancer.gov/about-cancer/treatment/types/immunotherapy [2] CAR T-cell Therapy and Its Side Effects. (n.d.). Retrieved March 30, 2022, from https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/immunotherapy/car-t-cell1.html [3] FDA-approved CAR T-cell Therapies | UPMC Hillman. (n.d.). UPMC HIllman Cancer Center. Retrieved March 31, 2022, from https://hillman.upmc.com/mario-lemieux-center/treatment/car-t-cell-therapy/fda-approved-therapies [4] Six years after CAR T-cell therapy for lymphoma, patient still cancer-free. (n.d.). Retrieved March 31, 2022, from https://www.uchicagomedicine.org/forefront/cancer-articles/a-walking-miracle-car-t-cell-therapy [5]Rebecca Borgert, P. (2021). Improving Outcomes and Mitigating Costs Associated With CAR T-Cell Therapy. Supplements and Featured Publications, 27(13). https://www.ajmc.com/view/improving-outcomes-and-mitigating-costs-associated-with-car-t-cell-therapy [6] Andrews, M. (2018, July 17). Staggering Prices Slow Insurers’ Coverage Of CAR-T Cancer Therapy. Kaiser Health News. https://khn.org/news/staggering-prices-slow-insurers-coverage-of-car-t-cancer-therapy/ [7] What Is Multiple Myeloma? (n.d.). Retrieved March 10, 2022, from https://www.cancer.org/cancer/multiple-myeloma/about/what-is-multiple-myeloma.html [8] New Drug Approval Moves Us Closer To Long-Term Control of Multiple Myeloma | Leukemia and Lymphoma Society. (n.d.). Retrieved March 10, 2022, from https://www.lls.org/blog/new-drug-approval-moves-us-closer-long-term-control-multiple-myeloma?utm_source=Instagram&utm_medium=Social&utm_campaign=3-2-2022-Myeloma-Drug-FDA-Approval-ZGM [9] New Data from CARTITUDE-1 Study Show Continued Deep and Durable Responses of Ciltacabtagene Autoleucel (cilta-cel) in Treatment of Heavily Pretreated Patients with Multiple Myeloma | Johnson & Johnson. (n.d.). Content Lab U.S. Retrieved March 10, 2022, from https://www.jnj.com/new-data-from-cartitude-1-study-show-continued-deep-and-durable-responses-of-ciltacabtagene-autoleucel-cilta-cel-in-treatment-of-heavily-pretreated-patients-with-multiple-myeloma [10] Chemotherapy Side Effects | American Cancer Society. (n.d.). Retrieved March 31, 2022, from https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/chemotherapy/chemotherapy-side-effects.html [11] Bishop, D. C., Clancy, L. E., Simms, R., Burgess, J., Mathew, G., Moezzi, L., Street, J. A., Sutrave, G., Atkins, E., McGuire, H. M., Gloss, B. S., Lee, K., Jiang, W., Maddock, K., McCaughan, G., Avdic, S., Antonenas, V., O’Brien, T. A., Shaw, P. J., … Micklethwaite, K. P. (2021). Development of CAR T-cell lymphoma in 2 of 10 patients effectively treated with piggyBac-modified CD19 CAR T cells. Blood, 138(16), 1504—1509. https://doi.org/10.1182/blood.2021010813