News Team member Stephanie Oehler describes how the online "trad-wife" aesthetic fuels the flames of the anti-vaccination movement during the second-largest measles outbreak of the 21st century.
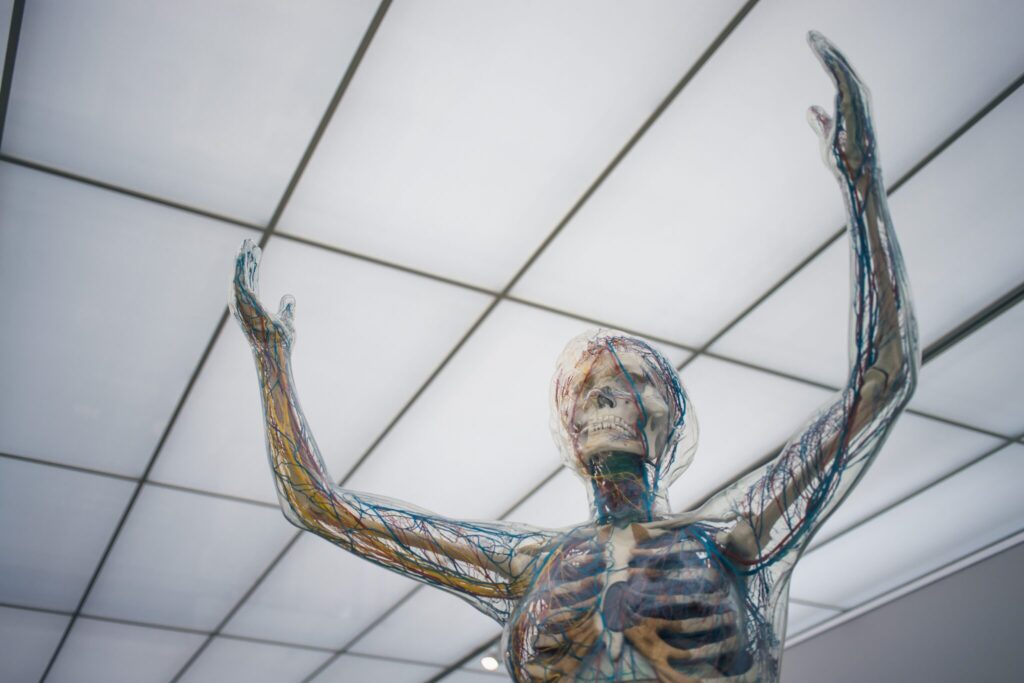
The human body is capable of keeping us alive through dire circumstances: disease, hunger, even extreme weather. The immune system — our body’s main defense against disease — plays an important role in keeping us healthy and alive. However, when the immune system malfunctions, it can allow the body to attack itself, resulting in the development of an autoimmune disease. A multitude of factors, on a genetic, individual, and societal level, can affect the development of autoimmune diseases, and a combination of these factors may help explain the stark rise in autoimmune diseases in the United States. With over 24 million Americans diagnosed with an autoimmune disease as of July 2021, the United States faces an increasingly dire autoimmune problem, and it is important that researchers investigate the root causes of these diseases.[1]
Autoimmunity is generally a mystery. While scientists understand that autoimmunity arises due to flawed immune system functioning, the cause behind this flaw remains unknown for most autoimmune diseases. Deciphering the main contributors to this flawed immune-system functioning may provide better prevention and treatment for autoimmune diseases in the future.
Our immune systems are meant to function like superheroes: They protect us from deadly diseases and allow us to build immunity against pathogens. There are many components of the immune system, the most important being macrophages, T cells, and B cells. When we are exposed to a pathogen, such as Covid-19, the macrophages in our body recognize it as an invader. The macrophage will engulf the threat and become an antigen-presenting cell, which is a way to signal the invasion to other cells and call for backup. The macrophage shows the T cells what the threat looks like so they can join the fight, similar to how multiple superheroes fight against one enemy. One type of T cell, the helper T cells, communicates the invasion of the pathogen to the B cells, which then produce antibodies whose job is to fight this specific pathogen. Another type, killer T cells, kill any cells that the pathogen has already taken over. This increase in immune cells creates inflammation which causes typical illness symptoms like fever, fatigue, and chills. After the threat has been eliminated, a third type of T cells, T regulatory cells, helps conclude immune response so the body can go back to normal. However, just as when one superhero fails to respond to the attack, when one part of the immune system does not function properly, a multitude of problems can occur.[2,3]
The etiology of the word autoimmune is self (auto) + resistant to disease (immune).[4] Just as in a movie in which the superhero turns out to be a villain, the body releases an immune response to itself, and mistakenly attacks healthy cells and tissues. In rheumatoid arthritis, for example, the body begins to recognize its own joints as foreign. The immune system releases a constant response attacking the joints because it falsely believes that the joints are invaders. This can cause debilitating symptoms such as pain, aches, and fatigue.[5]

More than 80 autoimmune diseases have been diagnosed in U.S. patients , the most common being rheumatoid arthritis, type 1 diabetes, lupus, celiac disease, and multiple sclerosis.[6, 7] Most autoimmune diseases are considered chronic diseases; while there may be treatments that ease symptoms and encourage longevity, they are often ‘incurable’ due to their mysterious origins. Scientists know that autoimmune diseases left untreated result in tissue and organ damage, and can be fatal. But the ability to predict the likelihood of developing an autoimmune disease remains unknown for most diseases due to the mysterious nature of how they arise.[8]
While the definitive cause behind the development of autoimmune diseases remains unknown, scientists do believe that most autoimmune diseases occur due to a mix of genetic and environmental factors, as well as chronic inflammation. Celiac disease, for example, has a genetic component, but this does not completely explain the development of the disease. In these cases, epigenetics, the interaction of genes with environmental factors, plays an important role.[9] In addition to genetics and epigenetics, scientists believe that the constant activation of the immune system causes chronic inflammation, which negatively impacts the functioning of organ systems throughout the body. This chronic inflammation may play a role in the development of autoimmune diseases due to the overactivation of the immune system –though it is unclear whether chronic inflammation plays a causal or resultant role.[10]
On an individual level, scientists theorize that environmental factors like nutrition and exercise level can affect autoimmune disease development. These environmental factors can affect the prevalence of the most common biomarker of autoimmunity, which is a type of antibody found in the blood called antinuclear antibodies (ANA).[11] In a recent study, researchers found that the prevalence of ANA has increased from 11% in 1988-1991 to 15.9% in 2011-2012.[12] This means that 4.9% more of the population had these antibodies in their blood in 2011 than they did in 1988. These results are thought-provoking because the researchers suggest that environmental changes, such as diet, exercise-level, and pollution among others, may play an important role in this increase.[13] These factors may help uncover the mystery of what can be done to prevent autoimmune diseases from developing.

On a societal level, it becomes apparent that some of the environmental risk factors for autoimmune diseases may be social determinants: race, gender, socioeconomic status, transportation access, and other social factors that affect health.[14] In a 2003 study published in Autoimmunity Reviews, researchers found that autoimmune diseases are one of the leading causes of death for young and middle-aged women in the U.S.[15] They also found that black people are more likely than white people to be diagnosed with several autoimmune disorders, and at a younger age.[16] Additionally, a 2014 study reports that socioeconomic status, a composite measure of income, education, and wealth, may be associated with worse physical and mental health after being diagnosed with certain autoimmune diseases, as well as a worse disease prognosis.[17] Taken together, this data suggests that disadvantaged groups may be more likely to have an autoimmune disease, which provides insight into a possible factor in autoimmune disease development.
As the mystery of autoimmune diseases is slowly uncovered, stark social inequality must be reckoned with. If environmental factors play as large a role as genetic factors in the development of autoimmunity, then the unequal access to preventative behaviors and care in the United States may cause unequal autoimmune disease diagnoses as well. Targeting equal access to environmental factors and social determinants of health may be an important pathway to curb the rise in autoimmunity and autoimmune disease diagnoses in the United States. Our immune systems are like superheros, but with the wrong mix of environmental and genetic factors, they can also be like villains.
References:
[1] National Institute of Environmental Health Science. (2021). Autoimmune Diseases. National Institute of Environmental Health Science (NIEHS). https://www.niehs.nih.gov/health/topics/conditions/autoimmune/index.cfm. [2] National Institute of Allergy and Infectious Disease. (2013). Immune System Research. National Institutes of Health (NIH). https://www.niaid.nih.gov/research/immune-system-overview. [3] Saldana, J. I. (n.d.). Macrophages. British Society for Immunology. https://www.immunology.org/public-information/bitesized-immunology/cells/macrophages. [4] Merriam-Webster. Immune Definition. https://www.merriam-webster.com/dictionary/immune. [5] Goldmuntz, E., and Penn, A. S. (2019. Autoimmune Diseases. U.S. Department of Health & Human Services: Office on Women’s Health. https://www.womenshealth.gov/a-z-topics/autoimmune-diseases. [6] National Institute of Environmental Health Science. (2021). Autoimmune Diseases. National Institute of Environmental Health Science (NIEHS). https://www.niehs.nih.gov/health/topics/conditions/autoimmune/index.cfm. [7] National Institute of Environmental Health Science. (2021). Autoimmune Diseases. National Institute of Environmental Health Science (NIEHS). https://www.niehs.nih.gov/health/topics/conditions/autoimmune/index.cfm. [8] National Institute of Environmental Health Science. (2021). Autoimmune Diseases. National Institute of Environmental Health Science (NIEHS). https://www.niehs.nih.gov/health/topics/conditions/autoimmune/index.cfm. [9] Jörg, S., Grohme, D. A., Erzler, M., Binsfeld, M., Haghikia, A., Müller, D. N., Linker, R. A., & Kleinewietfeld, M. (2016). Environmental factors in autoimmune diseases and their role in multiple sclerosis. Cellular and molecular life sciences : CMLS, 73(24), 4611—4622. https://doi.org/10.1007/s00018-016-2311-1 [10] Duan, L., Rao, X., & Sigdel, K. R. (2019). Regulation of Inflammation in Autoimmune Disease. Journal of immunology research, 2019, 7403796. https://doi.org/10.1155/2019/7403796 [11] National Institutes of Health. (2020). Autoimmunity may be rising in the United States. National Institutes of Health (NIH). https://www.nih.gov/news-events/news-releases/autoimmunity-may-be-rising-united-states. [12] Dinse, G.E., Parks, C.G., Weinberg, C.R., Co, C.A., Wilkerson, J., Zeldin, D.C., Chan, E.K.L. and Miller, F.W. (2020), Increasing Prevalence of Antinuclear Antibodies in the United States. Arthritis Rheumatol, 72: 1026-1035. https://doi.org/10.1002/art.41214. [13] Dinse, G.E., Parks, C.G., Weinberg, C.R., Co, C.A., Wilkerson, J., Zeldin, D.C., Chan, E.K.L. and Miller, F.W. (2020), Increasing Prevalence of Antinuclear Antibodies in the United States. Arthritis Rheumatol, 72: 1026-1035. https://doi.org/10.1002/art.41214. [14] Cooper, G.S., and Stroehla, B.C. (2003). The epidemiology of autoimmune diseases. Autoimmunity Reviews, 2(3): 119-125. https://doi.org/10.1016/S1568-9972(03)00006-5. [15] Cooper, G.S., and Stroehla, B.C. (2003). The epidemiology of autoimmune diseases. Autoimmunity Reviews, 2(3): 119-125. https://doi.org/10.1016/S1568-9972(03)00006-5. [16] Cooper, G.S., and Stroehla, B.C. (2003). The epidemiology of autoimmune diseases. Autoimmunity Reviews, 2(3): 119-125. https://doi.org/10.1016/S1568-9972(03)00006-5. [17] Calixto, O., and Anaya, J. (2014). Socioeconomic status: The relationship with health and autoimmune diseases. Autoimmunity Reviews, 13(6): 641-654. https://doi.org/10.1016/j.autrev.2013.12.002.